In a recent study, neuroscientists from Scripps Research discovered that targeting specific neurons involved in the brain’s stress response could potentially reduce alcohol consumption in individuals suffering from both post-traumatic stress disorder (PTSD) and alcohol use disorder (AUD). Published in Molecular Psychiatry, this research offers a promising direction for developing new treatment strategies for people grappling with these interlinked disorders.
Individuals with PTSD are at a heightened risk of developing AUD, often using alcohol as a coping mechanism to mitigate the symptoms of PTSD, such as anxiety, depression, and the distress from traumatic memories. This self-medication hypothesis suggests that alcohol may temporarily reduce the emotional pain and stress associated with PTSD, albeit with long-term negative consequences.
Existing pharmacotherapies to simultaneously address PTSD and AUD are scarce and often inadequate. The overlapping symptoms and mutual reinforcement of PTSD and AUD complicate treatment approaches, highlighting an urgent need for novel therapeutic strategies that can target both conditions effectively.
“Traumatic experiences in life can increase vulnerability to alcohol drinking and exacerbate symptoms of depression and anxiety,” explained senior author Marisa Roberto, the Schimmel Family Endowed Chair and vice chair of the Department of Molecular Medicine. “Alcohol is often used as a coping strategy to blur trauma-associated memories and diminish negative emotional states.”
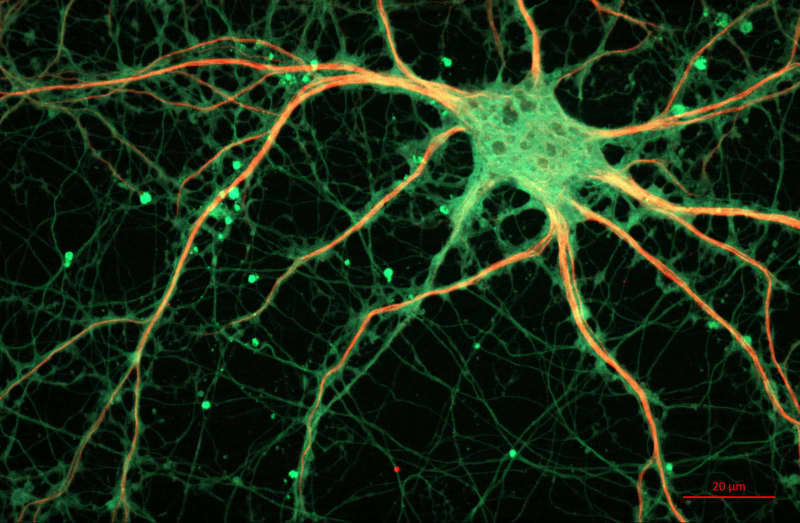
Prior research indicated that corticotropin-releasing factor (CRF) plays a crucial role in stress and alcohol drinking behaviors, particularly through its action in the central amygdala, a brain region involved in processing fear and stress responses. The new study aimed to investigate whether inhibiting CRF-expressing neurons in this region could reduce alcohol consumption in a rat model of comorbid PTSD and AUD, thereby identifying a potential therapeutic target.
Roberto’s team previously developed a rat model that mimics the symptoms observed in individuals with concurrent PTSD and AUD, including aggression, anxiety, heightened alertness, sleep disturbances, and elevated alcohol intake. In their new research, they compared these rats against a group that did not display these behaviors.
The study utilized a total of 121 Wistar rats, divided into groups to explore the effects of stress and subsequent alcohol consumption. The researchers employed a “2-hit” model that first exposed rats to a stress-inducing procedure followed by a period of voluntary alcohol consumption.
To induce stress, the rats underwent familiar footshock stress procedures in an inhibitory avoidance apparatus, designed to simulate traumatic events. This involved administering footshocks to the rats in a context that they could learn and remember, mimicking the way traumatic memories can trigger stress responses in humans.
Following the stress induction, all rats were given access to alcohol in a two-bottle choice setup, allowing them to choose between water and a 20% alcohol solution. This phase aimed to assess voluntary alcohol consumption post-trauma exposure.
Rats subjected to the stress induction procedure exhibited increased voluntary alcohol consumption compared to their unstressed counterparts. This finding aligns with the hypothesis that stress and trauma can escalate alcohol use, mirroring the patterns observed in individuals with comorbid PTSD and AUD.
To probe the neural underpinnings further, a subset of rats underwent a procedure to inhibit CRF-expressing neurons within the central amygdala through a chemogenetic technique, employing Designer Receptors Exclusively Activated by Designer Drugs (DREADDs). This approach allowed the researchers to selectively inhibit these CRF-producing neurons by administering a specific drug, thereby assessing the direct impact of CRF neuronal activity on alcohol consumption and stress-related behaviors.
The researchers found that inhibiting the activity of CRF-producing neurons in the central amygdala of stressed rats resulted in a marked decrease in alcohol consumption. This pivotal result suggests that CRF neurons in the central amygdala play a crucial role in mediating stress-induced alcohol use, offering a potential target for therapeutic interventions.
Interestingly, the inhibition of CRF-expressing neurons did not reduce anxiety-like behaviors in the rats, even though it decreased alcohol consumption. This observation indicates that while CRF activity in the central amygdala contributes to alcohol use in the context of stress, it may not be the sole mediator of anxiety and trauma-related behaviors.
“We were surprised to see that the anxiety phenotypes were not reduced when silencing CRF expressing neurons in the central amygdala, suggesting other neuropeptide co-factors might be at play,” said Bryan Cruz, the study’s first author and a postdoctoral fellow at Scripps Research.
While the study offers promising avenues for therapeutic intervention, it also acknowledges its limitations, including the need for further research to clarify the role of other neuropeptides and molecular systems involved in PTSD and AUD. The use of animal models, while invaluable, calls for cautious extrapolation of findings to human conditions, highlighting the necessity for continued exploration in diverse experimental settings.
Looking ahead, the researchers emphasize the importance of disentangling the specific neurological mechanisms underlying stress-related alcohol consumption and trauma-induced anxiety. This endeavor not only seeks to refine our understanding of these complex conditions but also to pave the way for innovative treatment strategies that can address the nuanced needs of individuals afflicted by the debilitating comorbidity of PTSD and AUD.
“Understanding the neurobiology of PTSD-AUD is key for development of future intervention strategies for this devastating comorbidity,” Roberto said. “We speculate that other neuropeptides with anti-stress properties may be involved in PTSD-AUD.”
The study, “Chemogenetic inhibition of central amygdala CRF-expressing neurons decreases alcohol intake but not trauma-related behaviors in a rat model of post-traumatic stress and alcohol use disorder,” was authored by Bryan Cruz, Valentina Vozella, Vittoria Borgonetti, Ryan Bullard, Paula C. Bianchi, Dean Kirson, Luisa B. Bertotto, Michal Bajo, Roman Vlkolinsky, Robert O. Messing, Eric P. Zorrilla, and Marisa Roberto.