In a study conducted by Weill Cornell Medicine scientists, a novel human neuron model has been developed that simulates the spread of tau protein aggregates in the brain. This phenomenon is a key driver behind cognitive decline observed in Alzheimer’s disease and frontotemporal dementia. The study, published in Cell00306-4), helps to identify potential targets for drug development that could block the spread of tau aggregates.
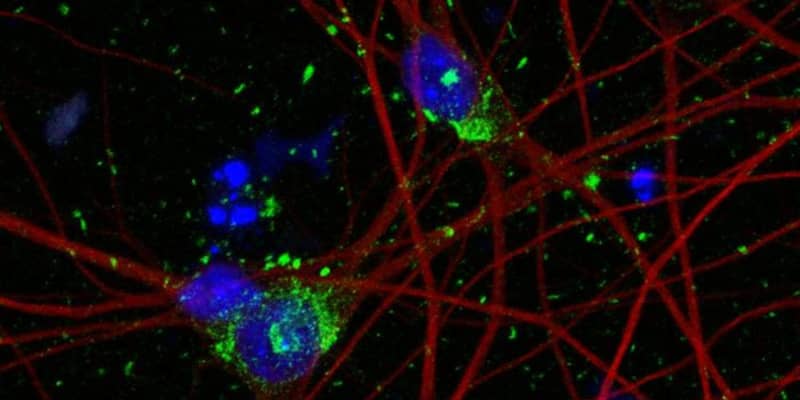
Tau aggregates are clumps of misfolded tau proteins that accumulate inside the neurons of the brain, disrupting their normal function and leading to cell death. These aggregates are a hallmark of several neurodegenerative diseases. In a healthy brain, tau proteins help stabilize microtubules, which are critical for maintaining the structure of neurons and for the transport of nutrients and other molecules within the cell.
However, in certain diseases, tau proteins undergo abnormal chemical changes, causing them to fold improperly and stick together, forming aggregates. Over time, these aggregates accumulate to form larger structures known as neurofibrillary tangles, contributing to the progressive cognitive decline seen in affected individuals.
Despite considerable research efforts, there are currently no therapies available that can halt or reverse the spread of tau aggregates in the brains of patients. This represents a significant barrier to effective treatment and ultimately a cure for these devastating conditions. To address this challenge, the research team aimed to develop a novel human neuron model that could more accurately simulate the spread of tau protein aggregates.
The researchers began with human pluripotent stem cells, which have the potential to develop into any cell type in the body, including neurons. They used CRISPR/Cas9 technology to introduce specific mutations into the genomes of these stem cells, causing them to express pathological forms of the tau protein similar to those observed in aging brains affected by neurodegenerative diseases.
Under normal conditions, modeling the propagation of tau aggregates in neurons derived from human pluripotent stem cells is challenging due to the slow, decades-long course of tau pathology in the human brain. To overcome this, the team employed a novel strategy. By genetically modifying the stem cells to express the diseased forms of tau, they created a neuron model in which tau spread could be observed within weeks, significantly accelerating the timeline for studying tau pathology.
A pivotal component of the study’s methodology was the use of CRISPRi screening. This technique allowed the researchers to temporarily “turn off” approximately one thousand genes in the neuron model to assess their role in tau spread. Through this large-scale screening, they identified 500 genes that significantly impacted the abundance of tau, indicating their potential role in the disease process.
“CRISPRi technology allowed us to use unbiased approaches to look for drug targets, not confined to what was previously reported by other scientists,” said one of the lead study authors, Celeste Parra Bravo, a neuroscience doctoral candidate in the Weill Cornell Graduate School of Medical Sciences.
Among the most significant discoveries from the CRISPRi screening was the involvement of the UFMylation cascade, a cellular process related to protein modification and signaling. The researchers found that altering this cascade could block tau propagation in their neuron model.
This finding was further validated through both in vitro experiments with human neurons and in vivo studies using mouse models, highlighting the potential of targeting the UFMylation cascade as a therapeutic strategy for neurodegenerative diseases.
“We are particularly encouraged by the confirmation that inhibiting UFMylation blocked tau spread in both human neurons and mouse models,” said paper co-author Dr. Shiaoching Gong, associate professor of research in neuroscience in the Appel Institute at Weill Cornell Medicine.
The human neuron model cannot fully mimic the complexities of aging neurons or account for interactions with other brain cells, such as microglia, which influence tau spread. But by unveiling the UFMylation cascade as a novel therapeutic target and identifying hundreds of genetic modifiers of tau abundance, the researchers have provided new tools and directions for the development of treatments for Alzheimer’s disease and related conditions.
“Currently no therapies can stop the spread of tau aggregates in the brains of patients with Alzheimer’s disease,” said lead study author, Li Gan, director of the Helen and Robert Appel Alzheimer’s Disease Research Institute and the Burton P. and Judith B. Resnick Distinguished Professor in Neurodegenerative Diseases in the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine. “Our human neuron model of tau spread overcomes the limitations of previous models and has unveiled potential targets for drug development that were previously unknown.”
“Our discoveries in human neurons open the door to developing new treatments that could truly make a difference for those suffering from this devastating disease.”
The study, “Human iPSC 4R tauopathy model uncovers modifiers of tau propagation,” was authored by Celeste Parra Bravo, Alice Maria Giani, Jesus Madero Perez, Zeping Zhao, Yuansong Wan, Avi J. Samelson, Man Ying Wong, Alessandro Evangelisti, Ethan Cordes, Li Fan, Pearly Ye, Daphne Zhu, Tatyana Pozner, Maria Mercedes, Tark Patel, Allan Yarahmady, Gillian K. Carling, Fredrik H. Sterky, Virginia M.Y. Lee, Edward B. Lee, Michael DeTure, Dennis W. Dickson, Manu Sharma, Sue-Ann Mok, Wenjie Luo, Mingrui Zhao, Martin Kampmann, Shiaoching Gong, and Li Gan.
